Emergency first aid
Checking vital functions.
As the most vital organs we consider th brain, the heart and the lungs. The respective vital functions are consciousness, circulation and breathing. A problem with any of these functions must be considered as lifethreatening.
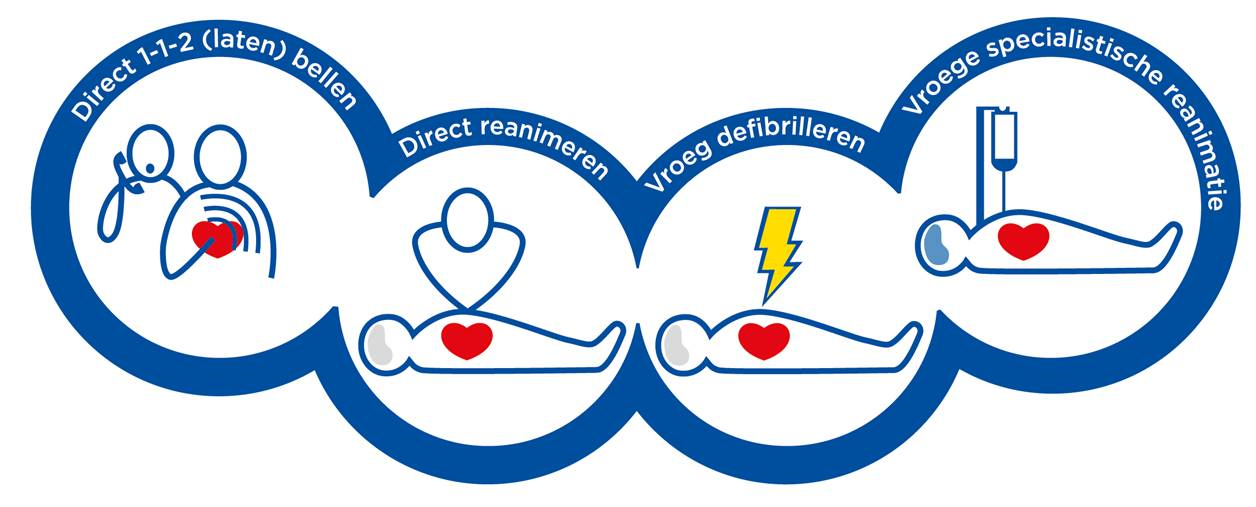
Checking these vital functions always happens according to a set protocol:
* check for consciousness by addressing the victim and gently shaking the shouders
* if a victim responds, try to find out what happened
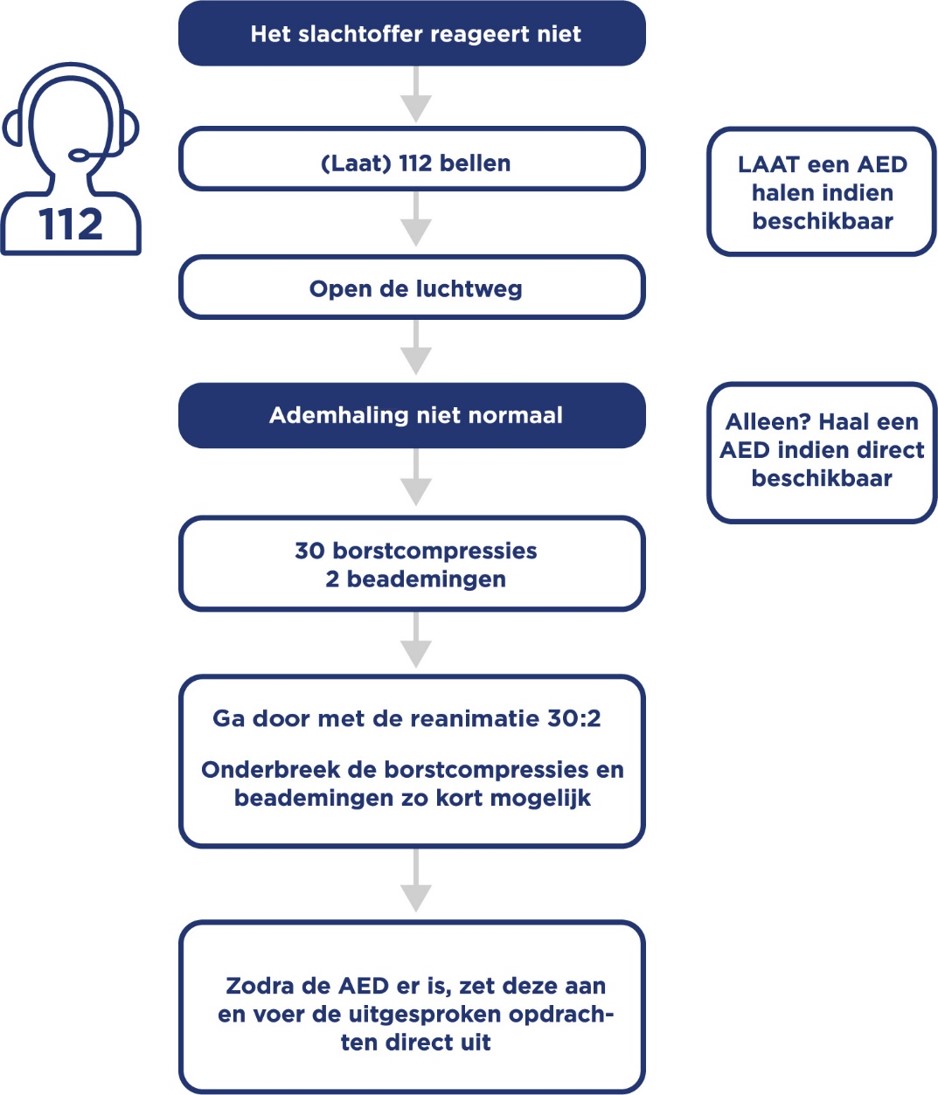
* if a victim does not respond, immediately call 1-1-2 or have someone else do this, and have someone fetch an AED if possible
* subsequently check the breathing of the victim
* if the victim is not breathing normally, alert the operator and immediately start CPR
Checking the consciousness.
Approach the victim on the side their face is pointing towards, and try to make contact.
Gently shake the victim by the shoulders and ask in a loud and clear voice "are you allright?"
Alert 1-1-2
When you call 1-1-2 on your mobile phone, first you will get the operator of the 'korps landelijke politiediensten'. He or she will ask what you need; ambulance, fire department or police and in which city. Then you will be connected to the regional emergy service. The operator there will ask for your name, telephone number and the address you are at.
After exchanging the necessary information and answering a few questions, you will proceed with checking the victim's breathing.
Checking the breathing.
* place one hand on the forehead of the victim and tilt the head slightly backwards
* use two fingers of the other hand to lift the chin a little bit to open the airway
* place your cheek over mouth and nose of the victim and listen and feel if there is any airflow
* at the same time look across the chest and abdomen of the victim to see if any movement is visible
* check for a maximum of 10 seconds
* if you do not observe any breathing, alert the operator and start CPR immediately
Attention!
The victim may show socalled agonal respiration. This is not normal breathing and is always a sign of a loss of cirrculation!
The victim makes abnormal breathing sounds, seems to be moaning or makes gurgling sounds.
Performing CPR
Performing chestcompressions
* place the heel of one hand on the middle of the sternum
* place the other hand on top of the first and lift the fingers of the first hand so they do not touch the chest
* depress the sternum 5 to 6 centimeters
* fully release the sternum, without losing contact with the chest
* perform 30 compressions at a rate of 100 to 120 per minute
Breathing
* place one hand on the forehead of the victim and tilt the head slightly backwards
* use two fingers of the other hand to lift the chin a little bit to open the airway
* using thumb and indexfinger of the hand which is on the forehead, close the nostrils of the victim
* place your mouth over the victim's and make sure you enclose it entirely
* breathe out during 1 secondinto the victim's mouth, and do this twice within 10 seconds
* at the same time watch from the corner of your eye, whether the victim's chest is rising
* turn your head away from the victim's face between the two breaths, so you can inhale fresh air
Connecting the AED
As soon as the AED arrives, it has to be connected as soon as possible. While doing this, interrupt the compressions as little as possible!
If you are alone and there is an AED nearby, then fetch and connect it first, then start CPR
With two EROs: work together as much as possible, so you have to interrupt CPR as little as possible
* depending on the type of AED, turn it on by pressing the button or opening the lid
* follow the instructions given by the AED accurately
* Every 2 munites the AED will analyse the victim's heartrate. This is an opportune moment to releave each other.
This way it is easier to continue CPR, especially when it takes a bit longer for professional assistance to arrive.